Abstract
Introduction:
Allogeneic hematopoietic cell transplantation (allo-HCT) is a curative option for several relapsed and refractory hematologic malignancies, including acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS). Success of allo-HCT lies in complete engraftment of donor hematopoietic cells and reconstitution of donor hematopoiesis. Among the well-defined factors of poor engraftment include HLA disparity between recipient and donor, T-cell-depleted grafts, reduced-intensity conditioning, and low stem cell dose. However, bone marrow reticulin fibrosis (MF) was not clearly defined as a risk factor.
Marrow fibrosis has not been observed to be associated with impaired engraftment in primary myelofibrosis patients undergoing allo-HCT. However, in patients with MDS a pre-existent MF showed a poor engraftment and secondary graft failure; Particularly, in patients with higher WHO grade fibrosis tend to have poor donor chimerism and transfusion dependency. But, this was not associated with any adverse effect on survival. Further studies have showed the time to neutrophil engraftment is prolonged in those with higher degree of MF but not in the lower grades. Studies evaluating these findings in AML with marrow fibrosis are lacking.
The current study is aimed at estimating the incidence of poor engraftment in AML/MDS patients with MF who underwent allo-HCT at our institution and to compare the incidence between those with and without MF.
Methods:
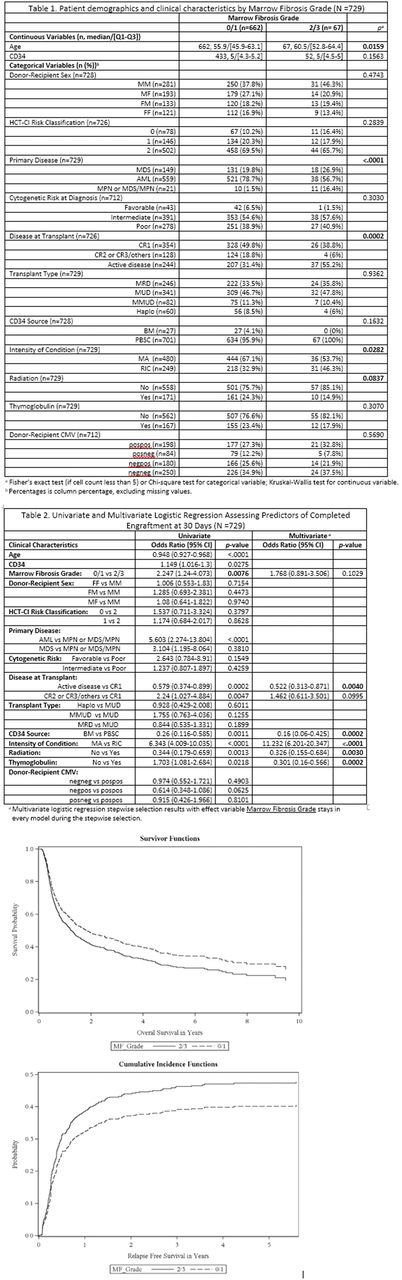
We retrospectively reviewed all AML/MDS patients that underwent allo-HCT between 2006 and 2015 at Washington University, St Louis. We included patients aged >18, and that underwent first allo-HCT. Patients that underwent second or later allo-HCT were excluded. Pre-transplantation bone marrows biopsies were evaluated for evidence of reticulin fibrosis and WHO grade (low grade/0-1, high grade/2-3) prior to allo-HCT. Primary end point was complete donor engraftment status measured using PCR based single-tandem repeats at day 30 post-allo-HCT. Secondary end point was to evaluate neutrophil engraftment, absolute platelet engraftment, day 100 engraftment status and survival outcomes. Neutrophil and platelet engraftment were defined per standard CIBMTR criteria.
The association between primary outcome and clinical risk factors was examine via univariate and multivariate logistic regression. The associations between neutrophil/platelet engraftment and clinical risk factors were examined via univariate and multivariate general linear modeling. The relationship between marrow fibrosis grade and overall survival, as well as competing risk survival of relapse and non-relapse mortality, was investigated by Cox proportional hazard regression.
Results:
Seven hundred and twenty-nine patients were included in the final analysis (grade 0/1 n=662; grade2/3 n=67) (Table 1). Patients in higher-grade fibrosis are relatively older (61 vs 56 years) are more likely to have MDS, likely to have active disease at transplantation (55% vs. 31%), and have had reduced intensity conditioning. Compared to patients with completed engraftment, patients in no-engraftment group are older (61.3 vs. 55.5; p= <0.0001) and a greater number of patients in that group have a higher grade of fibrosis (16% vs. 8%; p= 0.0064). Univariate analysis shows higher grade of MF is associated with engraftment failure at day 30 (odds ratio 2.247 95%CI 1.24-4.07; p= 0.008). However, in multivariate analysis, this significance was lost (odds ratio 1.77; CI 0.90-3.50; p= 0.10). MF grade was not associated with neutrophil and platelet engraftment, engraftment status at 100 days, overall survival, relapse free survival and non-relapse mortality. Factors associated with completed engraftment at day 30 post-allo-HCT are summarized in Table 2.
Conclusions:
Marrow fibrosis preceding allo-HCT was not associated with engraftment failure at day 30 or after transplantation with the adjustment for other risk factors.MF was not associated with other engraftment parameters or survival. Further analyses evaluating the effect of resolution of MF on survival outcomes is underway. It is imperative that several disease and transplantation characteristics play significant role than MF itself in engraftment failure supporting the theory that engraftment is an immunologic function.
Vij: Amgen: Honoraria, Research Funding; Abbvie: Honoraria; Takeda: Honoraria, Research Funding; Konypharma: Honoraria; Janssen: Honoraria; Bristol-Meyers-Squibb: Honoraria; Jazz: Honoraria; Celgene: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal